How to Lower High Blood Pressure Naturally with Food and Lifestyle (Evidence-Based Guide)

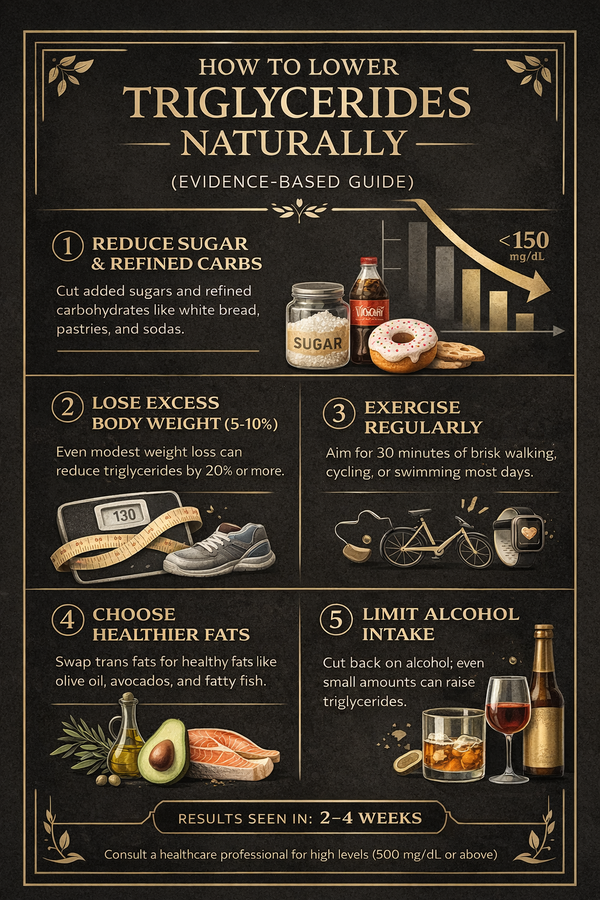
Meta Description High blood pressure is a “silent” risk factor for heart attack and stroke. Learn how to lower blood pressure naturally with evidence-based diet, movement, and lifestyle strategies. — How to Lower High Blood Pressure Naturally with Food and Lifestyle (Evidence-Based Guide) High blood pressure (hypertension) is often called a “silent killer.” It usually has no obvious symptoms, yet it quietly increases the risk of heart attack, stroke, kidney disease, and cognitive decline. Global estimates suggest that around 1.3–1.4 billion adults between 30 and 79 years old are living with hypertension, and only a minority have their blood pressure well controlled. The good news: for many people, targeted lifestyle changes can make a meaningful difference — sometimes as much as a single blood pressure pill — especially in the early and moderate stages. This guide explains what blood pressure actually is, why it matters, and which natural strategies have the strongest scientific support. > Important: This article is for general education only and does not replace personal medical advice. Never stop or change medication without discussing it with your healthcare provider. — What Is High Blood Pressure? Blood pressure is the force of circulating blood pushing against the walls of your arteries. It’s recorded as two numbers: Systolic (upper number): pressure when the heart contracts Diastolic (lower number): pressure when the heart relaxes between beats Many guidelines define high blood pressure in adults as 130/80 mmHg or higher, especially when readings are repeatedly elevated over time. Untreated hypertension accelerates damage to blood vessels and organs, increasing the risk of: Heart attack and heart failure Stroke Chronic kidney disease Vision problems Cognitive decline and dementia Because it usually feels “normal,” people can live with uncontrolled high blood pressure for years without realizing it. — Why Lifestyle Changes Matter Medications are often essential and lifesaving. But they work best when combined with healthy habits. Large research projects and clinical trials consistently show that changes in diet, activity, body weight, sodium intake, and alcohol use can: Lower systolic blood pressure (the top number) Improve long-term cardiovascular outcomes Sometimes reduce the amount of medication needed (under medical supervision) Think of lifestyle as “background pressure.” Drugs adjust the fine-tuning, but your daily habits set the baseline. — Evidence-Based Ways to Lower Blood Pressure Naturally 1. Follow a Blood-Pressure-Friendly Eating Pattern The most studied pattern for blood pressure is the DASH diet (Dietary Approaches to Stop Hypertension). It emphasizes: Plenty of vegetables and fruits Whole grains Beans, lentils, and nuts Low-fat dairy (if tolerated) Moderate amounts of fish and poultry Limited red and processed meats, sweets, and sugary drinks In controlled trials, the DASH pattern has lowered systolic blood pressure by around 5–6 mmHg and diastolic by around 3 mmHg in people with elevated blood pressure — even without weight loss. That might sound small, but on a population level, even a 2 mmHg drop in average systolic pressure can significantly reduce stroke and heart disease rates. — 2. Reduce Excess Sodium (Salt) — Sensibly Many people consume far more sodium than they realize, largely from: Restaurant and fast food Packaged sauces and instant noodles Processed meats and salty snacks Canned soups and ready meals Reducing sodium can lower blood pressure, especially in people who are “salt-sensitive” — common among older adults, people with hypertension, and those with kidney or metabolic issues. Practical steps: Cook more meals at home when possible. Taste food before salting; use herbs, spices, garlic, lemon, and vinegar for flavor. Choose “low-sodium” or “no added salt” versions of canned or packaged foods when available. Watch out for hidden sodium in sauces, instant seasonings, and processed meats. You don’t need a perfect 0-salt lifestyle. The goal is to move away from excessive sodium and heavily processed foods. — 3. Prioritize Potassium-Rich Whole Foods Potassium helps balance the effects of sodium and supports healthy blood vessel function. Many plant foods are naturally rich in potassium, such as: Leafy greens (spinach, Swiss chard, kale) Beans and lentils Potatoes and sweet potatoes (especially with skin) Bananas, oranges, and kiwis Tomatoes and tomato products without added salt For most people with healthy kidneys, increasing potassium from whole foods is beneficial. However, people with kidney disease or those on certain medications must be careful — always ask your doctor before making major changes. — 4. Maintain a Healthy Body Weight (Even Small Losses Help) Excess body weight, especially around the abdomen, increases blood pressure by: Making the heart work harder Worsening insulin resistance Promoting inflammation and hormonal changes that constrict blood vessels Research suggests that losing even 5–10% of body weight can lead to meaningful reductions in blood pressure and improvements in other risk factors. This does not require extreme diets. Instead, combine: Slightly reduced calorie intake More fiber and protein for fullness Reduced sugary drinks and ultra-processed snacks Regular movement (see next section) Slow, sustainable changes beat quick, aggressive weight-loss attempts that are hard to maintain. — 5. Move Your Body Most Days of the Week Physical activity makes blood vessels more flexible and improves how the body uses oxygen. Guidelines typically recommend: At least 150 minutes per week of moderate-intensity aerobic activity (for example, brisk walking, cycling, swimming) plus 2 sessions per week of muscle-strengthening activities (bodyweight exercises, resistance bands, or weights). In people with high blood pressure, regular aerobic exercise can lower systolic pressure by around 5–8 mmHg on average. Tips: Break it into small chunks (10–15 minutes) if longer sessions feel overwhelming. Walking is underrated: walking after meals is particularly helpful for both blood sugar and blood pressure. Choose activities you actually enjoy — consistency beats intensity. — 6. Limit Alcohol and Avoid Smoking Alcohol Even moderate drinking can raise blood pressure in some people. Reducing intake — or avoiding alcohol altogether — often leads to measurable improvements. Many experts suggest no more than one standard drink per day for women and two for men, with some people needing stricter limits or total avoidance (for example, those with uncontrolled hypertension or other conditions). Smoking Smoking briefly spikes blood pressure after each cigarette and damages blood vessels over time. Quitting doesn’t just lower cardiovascular risk; it also improves how well other blood-pressure treatments work. If quitting feels daunting, talk with a healthcare professional about support programs, medications, or nicotine-replacement options. — 7. Improve Sleep and Manage Stress Chronic stress and poor sleep keep the body in a “fight or flight” mode, raising stress hormones that constrict blood vessels and increase heart rate. Helpful practices: Aim for 7–9 hours of sleep per night, with consistent bed and wake times. Reduce screen exposure before bed and keep the bedroom dark and quiet. Experiment with simple relaxation tools: slow breathing, gentle stretching, short walks, or mindfulness practices. Stress management does not need to be mystical or perfect. Even small, regular moments of genuine relaxation can help. — How Quickly Can Blood Pressure Improve? Timeline varies, but research and clinical experience show patterns: Days to weeks: Reduced sodium intake Less alcohol More movement Often show early changes in blood pressure readings. Weeks to months: Consistent DASH-style pattern Weight loss Improved sleep and stress habits Typically produce more stable and sustained improvements. The earlier in the hypertension journey lifestyle changes are made, the more powerful they tend to be — but benefits can still occur later in life. — When Lifestyle Changes Are Not Enough Some people have strong genetic risk, long-standing hypertension, or other medical conditions where medication is essential from the start. Signals that you need professional help urgently include: Very high readings (for example, 180/120 mmHg or higher) Chest pain, shortness of breath, severe headache, or neurological symptoms (confusion, slurred speech, weakness on one side of the body) These situations are medical emergencies and require immediate care. For more typical high readings, your doctor may: Confirm with repeated measurements (including at home) Check for organ damage (heart, kidneys, eyes) Prescribe medication while also recommending lifestyle changes Lifestyle and medication are not rivals; they’re partners. — FAQ: Lowering Blood Pressure Naturally 1. Can I stop my blood pressure medication once my numbers improve? Possibly, but never on your own. Some people can reduce the dose or number of medications under medical supervision after consistent lifestyle changes and excellent readings. Others need long-term medication despite healthy habits. Only your healthcare provider can safely guide this. 2. Are salt substitutes safe for everyone? Many salt substitutes replace sodium with potassium. While they can help some people reduce sodium intake, they may be dangerous for those with kidney problems or on certain drugs (for example, ACE inhibitors, ARBs, or potassium-sparing diuretics). Always check with your doctor first. 3. Is coffee bad for blood pressure? Caffeine can cause a short-term rise in blood pressure, especially in people who are not used to it. For many regular coffee drinkers, the long-term impact is smaller. If you have high blood pressure, monitoring how your readings respond to your usual caffeine intake can be useful. 4. Do herbal supplements lower blood pressure? Some herbs and supplements are marketed for blood pressure, but evidence is often limited or mixed. More importantly, they can interact with medications. Focus first on proven lifestyle changes; discuss any supplement with a qualified healthcare professional. 5. What is a realistic goal? For many adults, a target below 130/80 mmHg is recommended, but the ideal goal depends on age, overall health, and other conditions. Your doctor can help define a safe and realistic target for you. — Final Thoughts High blood pressure is common — but it is not inevitable and not untouchable. By shifting daily habits toward: More vegetables, fruits, whole grains, and legumes Less sodium and fewer ultra-processed foods Regular movement Healthier body weight Limited alcohol, no smoking, and better sleep you can create a powerful “pressure-lowering” environment inside your body. Medications, when needed, build on that foundation. Together, they turn hypertension from a silent long-term threat into a manageable part of your health story, rather than the main character.