Omega-3, Fish, and Your Heart: Do You Really Need a Supplement?
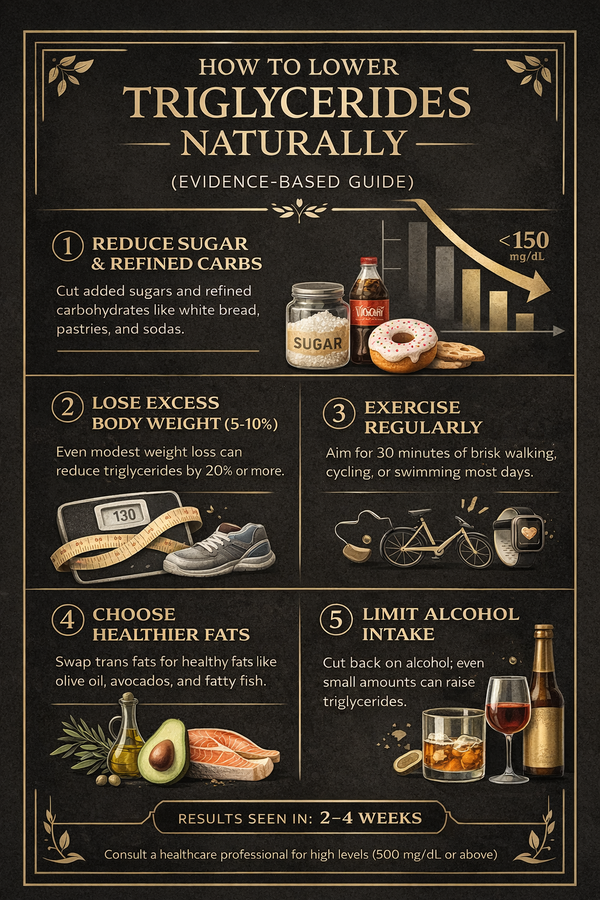
Omega-3 fats have been marketed as little capsules of heart protection for years. Fish oil lines the shelves, labels promise “cardio support,” and it can feel like you’re doing something good for your body every time you swallow one. Reality is more complicated. Omega-3 fats do play a real role in heart health — but how you get them (food vs supplements, dose, and context) matters far more than the marketing suggests. This guide walks through: What omega-3s actually are How they affect your heart and blood vessels What the evidence says about eating fish vs taking fish oil When supplements may help — and when they probably don’t — What Are Omega-3 Fatty Acids? Omega-3s are a family of polyunsaturated fats. The three main ones you’ll see: ALA (alpha-linolenic acid) – found in plants (flax, chia, walnuts, canola, soy). EPA (eicosapentaenoic acid) – mainly from marine sources (fatty fish, algae). DHA (docosahexaenoic acid) – also from marine sources; a key part of brain and retinal tissue. Your body can convert a small amount of ALA into EPA and DHA, but the conversion is inefficient. That’s why fatty fish (or algae-based products for strict vegetarians) are usually recommended for direct EPA/DHA intake. — How Omega-3s Support Heart Health Omega-3s affect several pathways that are important for cardiovascular disease: 1. Lowering triglycerides EPA and DHA consistently reduce blood triglyceride levels, especially at higher doses. 2. Improving non-HDL cholesterol profile Meta-analyses show a near-linear relationship between omega-3 intake and reductions in triglycerides and non-HDL cholesterol (a measure of all “bad” particles). 3. Anti-arrhythmic and membrane effects Omega-3s are incorporated into cell membranes in the heart and blood vessels, influencing electrical stability and possibly reducing some arrhythmia risks in specific settings. 4. Anti-inflammatory and endothelial effects They can shift the balance of signaling molecules toward less inflammatory profiles and may improve endothelial function (the inner lining of blood vessels). Taken together, these mechanisms explain why omega-3s have been such a big research target for preventing heart disease. — The Strongest Evidence: Eating Fish, Not Swallowing Capsules Observational and Advisory Data Large cohort studies and science advisories consistently find that eating fish 1–2 times per week — especially fatty fish like salmon, mackerel, sardines, and herring — is linked with lower risks of: Coronary heart disease Ischemic stroke Sudden cardiac death On the basis of this and other evidence, the American Heart Association (AHA) recommends that adults eat two servings of fish (particularly fatty fish) per week, roughly 3 oz cooked per serving. In simple terms: > People who regularly eat non-fried, fatty fish a couple of times a week tend to have fewer fatal heart events than those who rarely eat fish. Fish also brings other nutrients to the table (protein, vitamin D, selenium) that may add to this benefit. The whole food seems to matter more than any single isolated component. — What About Fish Oil Supplements? Here’s where things get more nuanced. 1. Mixed Results Across Trials Randomized controlled trials of omega-3 supplements have produced mixed results: A 2021 meta-analysis of 38 RCTs found that omega-3 fatty acids, overall, reduced cardiovascular mortality and improved outcomes, with stronger effects for EPA-only formulations compared with combined EPA+DHA. Other large analyses show modest or no benefit for broad, unselected populations, especially when low doses are used and background medical therapy (like statins) is already strong. Bottom line: Supplements are not a magic shield for everyone, but certain high-risk groups may benefit. — 2. High-Risk Patients and High Triglycerides Some of the clearest benefits appear in patients with cardiovascular disease and elevated triglycerides who receive high-dose prescription EPA: Trials like REDUCE-IT (using icosapent ethyl, a purified EPA product) showed significant reductions in cardiovascular events in patients with established CVD or diabetes plus additional risk factors, on top of statin therapy. In these settings, omega-3 therapy is acting more like a targeted drug than a general wellness supplement. — 3. Potential Risks: Atrial Fibrillation and Bleeding More recent work has raised safety questions about high-dose marine omega-3 supplements: Meta-analyses of cardiovascular outcome trials found that marine omega-3 supplementation was associated with an increased risk of atrial fibrillation (AF), particularly at higher doses. AF itself raises the risk of stroke and heart failure. This doesn’t mean omega-3 supplements are “bad,” but it does mean: High-dose fish oil is not something to start casually, especially if you already have arrhythmia risk, are on blood thinners, or have other complex health issues. Decisions about prescription-strength omega-3 should be made with a cardiologist or lipid specialist. — 4. Supplements vs Food: Why Food Usually Wins Most expert groups now emphasize: Food first – 1–2 servings of fatty fish per week for the general population. Supplements only when there’s a clear reason (for example, very high triglycerides, established CVD with specific risk profiles, or inability to eat fish), and ideally as prescription products with quality control. Supplements can lower triglycerides, but for many people they don’t clearly reduce heart attack or stroke risk beyond what you get from an overall healthy lifestyle — and they may slightly increase AF risk at high doses. — How Much Fish Should You Eat for Heart Health? Most guidelines converge on: At least 1–2 servings (about 8 oz / 225 g total) of fish per week, emphasizing fatty fish for omega-3 content. Good options: Salmon Sardines Mackerel Herring Trout Anchovies Tips: Prefer baked, grilled, steamed, or lightly pan-fried fish rather than deep-fried versions. If mercury is a concern (e.g., for pregnant people), choose lower-mercury species like salmon, sardines, and trout more often. If you absolutely don’t eat fish, algae-based DHA/EPA or carefully chosen supplements can be considered with professional guidance. — Practical Omega-3 Game Plan for Your Heart You don’t need a lab coat and a calculator. Try this simple pattern: 1. Base your diet on heart-healthy foundations Vegetables, fruits, whole grains, beans, nuts, and seeds Limited ultra-processed foods, sugary drinks, and processed meats 2. Add fish 1–2 times per week Swap one red-meat dinner for salmon. Keep canned sardines, tuna (in water or olive oil), or mackerel as easy backups. 3. Use plant omega-3s as support, not replacement Add ground flaxseed or chia to oatmeal or yogurt. Snack on a small handful of walnuts. 4. Talk to your clinician if you have high triglycerides or existing heart disease You may be a candidate for prescription-strength omega-3 (often EPA-only), but this needs a proper risk–benefit discussion. — FAQ: Omega-3, Fish Oil, and Heart Health 1. If I already eat fish twice a week, do I still need a supplement? For many people, no. If you regularly eat fatty fish and have no special risk factors, extra capsules rarely add proven benefit and may slightly increase AF risk at high doses. Food-based omega-3 intake plus an overall heart-healthy pattern is usually enough. — 2. I don’t like fish. Is flaxseed oil or chia enough for my heart? Plant sources (ALA) are helpful but don’t fully replace EPA/DHA. Some people choose algae-based EPA/DHA products instead of fish. If you avoid all fish, it’s worth discussing your overall risk profile and whether an EPA/DHA source makes sense. — 3. Can I just take a huge dose of fish oil and eat whatever I want? No. Omega-3s are not a cancel button for an otherwise high-risk lifestyle. The biggest benefits come when they’re layered on top of a healthy pattern (good blood pressure, no smoking, reasonable weight, high-fiber diet, movement) — not used as a shortcut. — 4. Are “triple-strength” or “pharmaceutical-grade” fish oils better? Higher-concentration products are useful to reach therapeutic doses for very high triglycerides with fewer capsules, but that doesn’t mean they’re appropriate for everyone. For general prevention, mega-doses are not automatically better and may increase AF risk. — 5. What’s a realistic first change I can make this month? For most people: > Add one fatty-fish meal per week and cut one ultra-processed, fried, or fast-food meal. You’ll increase omega-3s and improve overall diet quality in a single move. — Key Takeaways Omega-3s (especially EPA and DHA) support heart health, mainly by lowering triglycerides and influencing inflammatory and electrical pathways. The strongest and most consistent evidence is for eating fish 1–2 times per week, not for everyone taking fish oil pills. Supplements can be useful in specific high-risk scenarios, especially high triglycerides and certain CVD patients, usually under medical supervision. High-dose marine omega-3 supplements may increase atrial fibrillation risk, so more is not always better. Viewed this way, omega-3s stop being magic capsules and become what they really are: one meaningful piece of a broader, food-centered strategy to keep your heart’s pipes clear and its rhythm steady over the long haul.